Is Health Data Portability and Interoperability Within Reach… Globally?
In the summer of 2019, I had the opportunity to attend an Interoperability Summit in Seattle. A friend and former colleague had invited me, and I figured what better way to spend a couple of days, catching up with a long-time friend and meeting with industry leaders to discuss healthcare data interoperability. At the time, I was working for an organization that was attempting to build a cancer information system that brought together EMR, lab, pathology, genomic, and other data sets, and I was hoping to gain a few nuggets of insight that could help my team.
A central tenet of the summit was the premise that a patient should have access to all of the information that is relevant to their care and be able to share that data with the clinician of their choice to inform the best decisions for that individual’s care. The presenters discussed the need for standards, the challenges and barriers of interoperability – how to deal with legacy systems, semantic interoperability, and complicated data exchange regulations – and the many use cases demonstrating the value of interoperability. These use cases centered around aggregating data from a multitude of systems to create that ever-elusive comprehensive longitudinal health record to enable:
Coordination of care for patients
Understanding of an individual's social determinants of health
Clinical insights powered by AI
I walked away from that summit energized by the passion of the group, but also, having spent a fair amount of my career building solutions that enabled interoperability, with the distinct feeling that I had been having similar conversations for the past 10 years. Don’t get me wrong, a ton of progress had been made on standards and interoperability, but we were still seemingly looking for a unifying use case that was going to really push things forward by leaps and bounds.
That seems like a lifetime ago, as a few months after the summit I decided to join an organization focused on providing healthcare solutions to underserved communities in low-and middle-income countries. And then a few months after that, the pandemic hit.
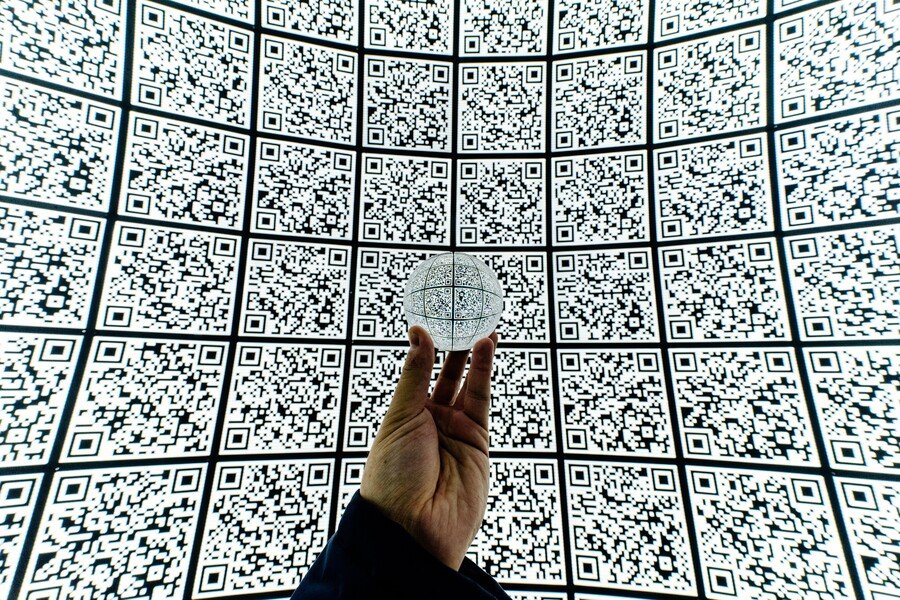
Out of sheer necessity, innovation in healthcare accelerated, as seen by the incredible advances in diagnostic testing, telemedicine, and development of vaccines and novel therapies. As vaccines were widely rolled out, there was a sudden need to easily share your vaccination status to get back to our pre-pandemic activities. And so came the concept of the SMART Health Card, a secure QR code that many of us have downloaded and used to show COVID-19 vaccination status. These health cards are currently used in ~25 states and are starting to proliferate worldwide. Is this not a prime example of health data portability and interoperability?
Yes, I understand, a COVD-19 vaccination record is a far cry from a longitudinal clinical record, much less one for an individual with a complicated medical history. But it is a START at a possible means of creating a portable record that enables seamless, personalized care anywhere. When I think about it in the context of underserved communities in the Global South – which in many areas are in the early stages of implementing digital systems – perhaps this offers a greenfield opportunity. An opportunity to build out systems that are centered around the basic principle that a patient should have access to all of the information that is relevant to their care and be able to easily control with whom, how, and when that information is shared.
Originally posted on Linkedin.